Related Articles
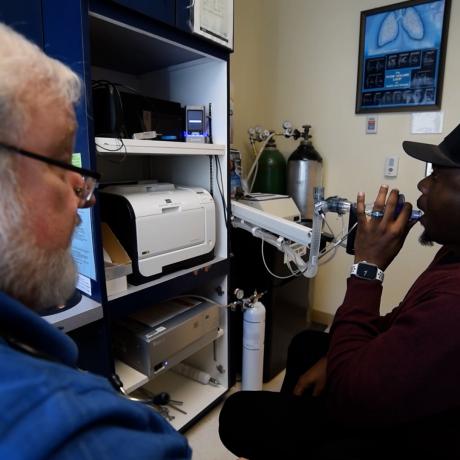
Two new educational videos now available from the National Rural Health Resource Center highlight the prevalence of chronic obstructive pulmonary disease (COPD) in the country’s rural communities and the steps that critical access hospitals and other small rural hospitals can take to improve access to much-needed pulmonary rehabilitation services.
Scott Daniels, the longtime Medicare Rural Hospital Flexibility (Flex) Program coordinator at the Hawaii Department of Health, Office of Primary Care and Rural Health, was awarded the 2023 Calico Quality Leadership Award at the annual Flex Program Reverse Site Visit held in Washington, DC on July 19-20.
The summit convened nationally recognized content experts in rural health care policy, health equity, value-based care, and clinical quality to explore the small rural hospital and rural health clinic’s roles in achieving health equity. Panelists focused on actionable steps on how to maximize available resources and data, and provide solutions for achieving rural health equity.
Teryl Eisinger, Advisor, National Organization of State Offices of Rural Health (NOSORH) was awarded the Calico Quality Leadership Award at the 2022 Flex Program Reverse Site Visit held virtually July 19-22, 2022.
The Delta Regional Authority announced 11 additional facilities chosen to participate in the Delta Region Community Health System Development (DRCHSD) Program.