Pinckneyville Community Hospital (PCH), located in Pinckneyville, Illinois, is one of just three critical access hospitals (CAHs) that received national recognition for demonstrating an innovative approach to post-acute care that supports a patient’s continued recovery from illness or management of a chronic illness or disability.
To better serve their patient population, PCH implemented the position of a transitional care management (TCM) nurse. This nurse functions to improve the care of the patient after they are discharged from the hospital. All high-risk patients about to be discharged are referred to the TCM nurse. The TCM nurse visits the patient while they are still in the hospital to explain the TCM process and answer any questions. Within forty-eight hours of being discharged, a phone call to check on the patient is made and a follow-up home visit is scheduled. Medication education and a review of the discharge instructions for comprehension are performed during this home visit.
The TCM nurse continues to make weekly phone calls for the next three weeks to check on the patient. The TCM nurse makes weekly updates to the primary care office and will work with the primary care provider or the home health agency to address any needs that are identified during the interactions with the patient. After 30 days of TCM, there is a warm handoff to the chronic care nurse for long-term management.
Positive Outcomes
- Readmissions rates for Pinckneyville have been reduced from 12.6 percent to 3.1 percent through the use of a dedicated TCM nurse and improved communication between all the team members.
- Pinckneyville Community Hospital is part of an accountable care organization (ACO) and is therefore cognizant of the need to control its skilled nursing facility (SNF) per member per month (PMPM) costs. Between Quarter 2 2019 and Quarter 1 2020, they have reduced their SNF PMPM spending from $97 to $90.
Top Accomplishments
The focus on transitional care management has clearly been an innovative approach for post-acute care. In addition to decreasing readmission rates and SNF PMPM costs, Pinckeyville’s initiatives have benefited their patient’s post-acute experiences in numerous ways. To decrease confusion over discharge medications, Pinckneyville Community Hospital created discharge medication instruction sheets. The instruction sheets were created through a collaboration between Pinckneyville’s pharmacists and hospitalists. The sheets increase patient understanding and therefore reduce medication errors. Both patient and physician satisfaction scores have improved since the implementation of the discharge medication instruction sheets. Moreover, all follow-up appointments for patients are scheduled prior to discharge. If the patient is discharged after hours, the clinic Care Coordinator calls and schedules an appointment time with the patient. This has greatly reduced missed appointments and helps to ensure continuity of care post-discharge.
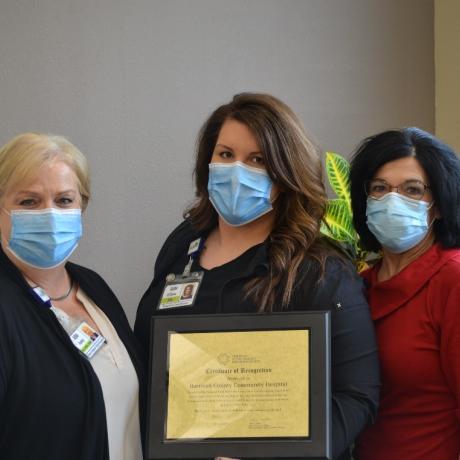
“With the addition of Barb Brand, RN, Transitional Care Coordinator, we have been able to reduce our readmission rate from 12.6 to 3.1. Barb assists with patients who are high-risk for readmission to ensure they understand their hospital discharge instructions, obtain their medications, keep their scheduled doctor’s appointments, and help coordinate any additional services they may need,” said Randall Dauby, CEO of Pinckneyville Community Hospital. “Barb works closely with Deb Hale, RN, Chronic Care Manager at Family Medical Center, to transition these patients to their primary care physician for further monitoring of their medical condition and implementing preventative care measures to keep the patient in their home setting.”
Laura Fischer, Flex Grant Project Manager from the Illinois Critical Access Hospital Network (ICAHN), said, “Illinois is very proud to have a critical access hospital doing such innovative work to provide comprehensive quality health care to its patients.”