Downloads
UPMC Susquehanna Muncy One-page Summary (723.77 KB)
Related Articles
Grant Memorial Hospital is recognized for demonstrating an innovative approach to collaboration through telehealth. They have successfully minimized barriers by connecting rural populations to needed health care to address clinical issues and patient needs, as well as provide support, resources, and education in behavioral health and cardiology.
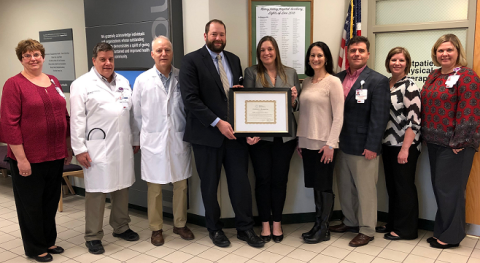
UPMC Cole, located in Coudersport, Pennsylvania, is one of three critical access hospitals CAHs that received national recognition for demonstrating an innovative approach to post-acute care that supports a patient’s continued recovery from illness or management of a chronic illness or disability.
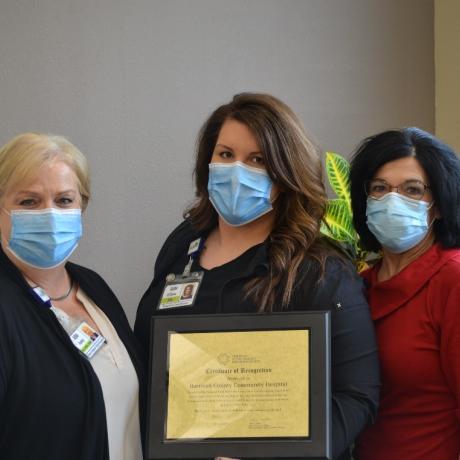
Harrison County Community Hospital (HCCH), located in Bethany, Missouri, is one of three critical access hospitals (CAHs) that received national recognition for demonstrating an innovative approach to post-acute care that supports a patient’s continued recovery from illness, or management of a chronic illness or disability.
Pinckneyville Community Hospital, located in Pinckneyville, Illinois, is one of just three critical access hospitals that received national recognition for demonstrating an innovative approach to post-acute care that supports a patient’s continued recovery from illness or management of a chronic illness or disability.
Lexington Regional Health Center (LRHC), located in Lexington, Nebraska, was one of only four CAHs that received national recognition for demonstrating innovative care coordination initiatives to improve population health.