Featured Stories
Article Type
Programs
45 results found
Sakakawea Medical Center (SMC) was recognized for their innovative efforts connected to care coordination. In January 2015, SMC created a new position to facilitate care coordination efforts between the hospital and other care providers in the community.
With assistance from the North Carolina SORH, Vidant Chowan Hospital implemented a ‘No Patient Left Behind’ transitional health program, a free service through which patients with chronic obstructive pulmonary disease, diabetes, post-acute AMI, congestive heart failure and pneumonia are helped to transition back to their home upon discharge.
Carondelet Holy Cross Hospital was recognized for innovation in emergency medical services (EMS). In 2014, health care providers serving residents of Santa Cruz County, Arizona, came together to create the Community Healthcare Integrated Paramedicine Project (CHIPP).
Gunnison Valley Hospital implemented a process of bedside reporting. Reporting nurses finishing and starting a shift meet with the patient to give report on current treatment plans and to address any questions or concerns. An emphasis is placed on talking with the patient rather than about the patient.
In response to the high levels of mental health needs and the challenge of limited resources, Athol Hospital partnered to develop a collaborative school-based telepsychiatry model focused on bridging care gaps for children and families residing in the Athol Hospital service area.
In conjunction with another hospital, Pender Memorial Hospital successfully implemented the Transitions in Care program. The program provides telehealth for congestive heart failure patients to assist with self-managing cardiac disease, reducing readmissions and encouraging independent living for seniors.
Sanpete Valley Hospital worked with Intermountain Healthcare to create a network that provides appropriate access to behavioral health, working within the community to educate about mental health issues, increase access to care, provide timely access to services and improve follow-up with patients.
Estes Park Medical Center (EPMC) was recognized for its work in the areas of care coordination, care management, patient access and prevention and wellness projects. EPMC joined a public-private partnership to form a wellness center that provides an array of services to the community.
McKenzie Health System received recognition for working on key projects such as the Patient Centered Medical Home (PCMH) model to develop a deeper relationship with patients and develop skills to improve patient health through evidence-based medicine techniques to manage chronic disorders.
Illini Community Hospital has implemented a care coordination program that consolidates management of populations into one seamless system, producing efficiencies that drive improved health outcomes and reduce overall health care spending.
Moab Regional Hospital (MRH) was recognized for turning their financial crisis in 2011 to financial success in 2013. A number of factors contributed to the success of MRH’s turnaround, including re-participating in the Disproportionate Share Hospital (DSH) program and conducting a CHNA to better address the community’s health needs.
The dramatic turnaround at Pershing General Hospital began with a top-to-bottom facility assessment by hospital administration of unprofitable service lines and a comprehensive review of community health needs.
Blue Mountain Hospital was recognized for implementing many programs to communicate with the community they serve, including a county newsletter and social media engagement. These communication methods are all utilized to maintain open lines of communication with the community.
Decatur County Memorial Hospital reached out to its community in several ways including free influenza vaccines for the community and free comprehensive blood screenings at the county health fair. By partnering, the hospital and Decatur County came together to enhance the overall health of their community.
Mason District Hospital provides integrative care that meets the needs of each patient through the Integrated Health Advocacy Program (IHAP), a chronic disease management program that supports and educates participants and provides whole person care in an effort to improve health and quality of life, while decreasing health care costs.
Ellenville Regional Hospital was recognized for their effort in community engagement with the creation of a seamless process of medication management as patients transition within and across organizations.
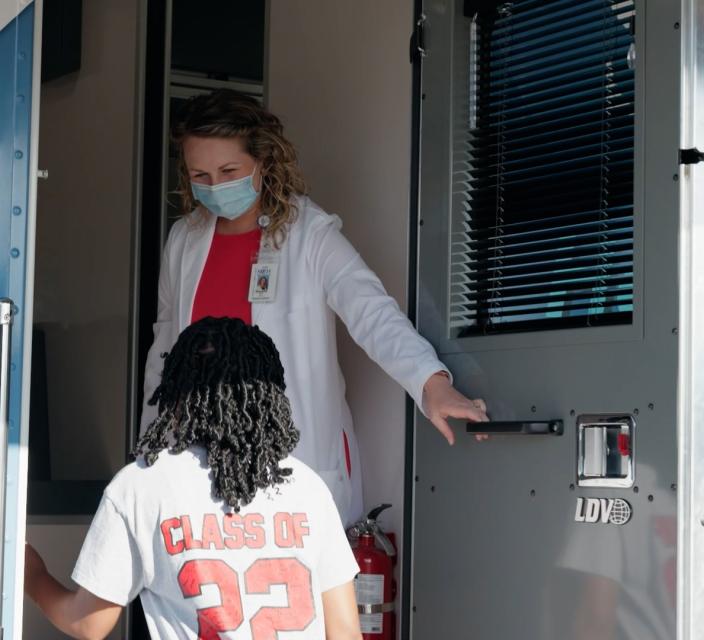
Granite County Medical Center spearheaded the effort to establish a mobile dental clinic where the nearest dentist can be up to 70 miles away. GCMC helped with billing, scheduling, marketing, housekeeping, fundraising, IT support, administrative support, and maintenance.
Central Valley Medical Center (CVMC) demonstrated excellence in quality initiatives with improvements in patient safety and satisfaction. CVMC was one of the first CAHs in Utah to report quality measures and has continued to lead by example
Tahoe Forest Hospital District was recognized for their quality reporting strategies and demonstrated excellence in quality initiatives with documented outcomes.
Page Hospital participated in the CMS Partnership for Patients initiative through the Premier Hospital Engagement Network (HEN). The hospital maintained Joint Commission accreditation and demonstrated high quality outcomes and operational performance rates relative to peers.