Awardees
Grant Memorial Hospital is recognized for demonstrating an innovative approach to collaboration through telehealth. They have successfully minimized barriers by connecting rural populations to needed health care to address clinical issues and patient needs, as well as provide support, resources, and education in behavioral health and cardiology.
UPMC Cole, located in Coudersport, Pennsylvania, is one of three critical access hospitals CAHs that received national recognition for demonstrating an innovative approach to post-acute care that supports a patient’s continued recovery from illness or management of a chronic illness or disability.
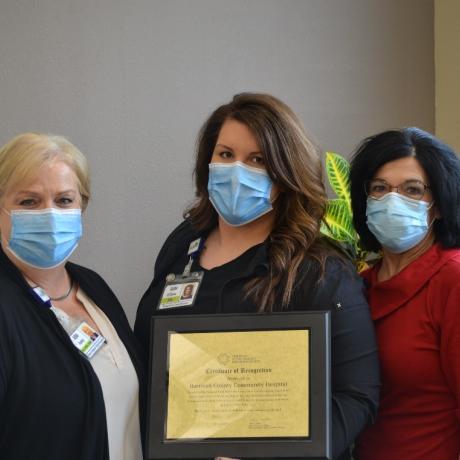
Harrison County Community Hospital (HCCH), located in Bethany, Missouri, is one of three critical access hospitals (CAHs) that received national recognition for demonstrating an innovative approach to post-acute care that supports a patient’s continued recovery from illness, or management of a chronic illness or disability.
Pinckneyville Community Hospital, located in Pinckneyville, Illinois, is one of just three critical access hospitals that received national recognition for demonstrating an innovative approach to post-acute care that supports a patient’s continued recovery from illness or management of a chronic illness or disability.
Lexington Regional Health Center (LRHC), located in Lexington, Nebraska, was one of only four CAHs that received national recognition for demonstrating innovative care coordination initiatives to improve population health.
Lincoln County Medical Center (LCMC), located in Ruidoso, New Mexico, was one of only four CAHs that earned national recognition for demonstrating innovative care coordination initiatives to improve population health.
Mason District Hospital, located in Havana, Illinois, is one of only four CAHs across the United States to receive national recognition for its care coordination program.
Ste. Genevieve County Memorial Hospital (SGCMH), located in Ste. Genevieve, Missouri, is one of only four CAHs that received national recognition for demonstrating innovative care coordination initiatives to improve population health.
Ellenville Regional Hospital is recognized for implementing an innovative project to fight the opioid crisis in collaboration with a federally qualified health care center (FQHC). The Opiate Reduction Medicaid Accelerated Exchange Series Pilot (Max) Project has provided a new model of care in an effort to decrease the administration of opioids in the Emergency Department (ED).
Margaretville Hospital is recognized for an innovative mental health program for students that combines in-person psychotherapy and telepsychiatry in public schools at no cost to the students, their families, or the school district.
Columbia Basin Hospital, Columbia County Health System, Jefferson Healthcare, Newport Hospital and Health Services, Pullman Regional Hospital, and Whitman Hospital and Medical Center are recognized for an innovative, multi-state, rural palliative care initiative that includes telehealth case consultation with an interdisciplinary team.
Boulder City Hospital is recognized for the use of Project ECHO to advance the quality of their antibiotic stewardship program.
UPMC Susquehanna Muncy is recognized for the development of innovative telehealth services, including stroke.
River Hospital is recognized for demonstrating innovation in the integration of behavioral health initiatives.
Fulton County Medical Center (FCMC) is being recognized for the development of an innovative emergency department (ED) mental health distress response.
Union General Hospital was recognized for the development of innovative programs, It's a Girl Thing and Together We Can Be Bully Free, geared toward awareness of adolescent behaviors and how to change them.
Tillamook Regional Medical Center was recognized for implementing an innovative Community Paramedic program in their county.
Hansford County Hospital District collaborated with Northwest Central Texas EMS Resources, Inc. to create a program that arms registered nurses with the knowledge and training of an emergency medical technician with a class titled RN to Basic.
Avera Holy Family Hospital partnered with four emergency medical service EMS programs, the police department, and public health in a three-year continuous quality improvement project. This project engaged EMS and hospital systems of care with collaborative prevention initiatives, data collection and evaluation, ongoing protocol development, and training.
Good Shepherd Medical Center implemented an immensely successful care coordination program, called Healthy Living Communities, to help senior citizens live healthy lives in the community. The Health Living Communities program staff, including nurses and community health workers (CHWs), masterfully connected community resources with health care teams.
Sakakawea Medical Center (SMC) was recognized for their innovative efforts connected to care coordination. In January 2015, SMC created a new position to facilitate care coordination efforts between the hospital and other care providers in the community.
With assistance from the North Carolina SORH, Vidant Chowan Hospital implemented a ‘No Patient Left Behind’ transitional health program, a free service through which patients with chronic obstructive pulmonary disease, diabetes, post-acute AMI, congestive heart failure and pneumonia are helped to transition back to their home upon discharge.
Gunnison Valley Hospital implemented a process of bedside reporting. Reporting nurses finishing and starting a shift meet with the patient to give report on current treatment plans and to address any questions or concerns. An emphasis is placed on talking with the patient rather than about the patient.
Carondelet Holy Cross Hospital was recognized for innovation in emergency medical services (EMS). In 2014, health care providers serving residents of Santa Cruz County, Arizona, came together to create the Community Healthcare Integrated Paramedicine Project (CHIPP).
In response to the high levels of mental health needs and the challenge of limited resources, Athol Hospital partnered to develop a collaborative school-based telepsychiatry model focused on bridging care gaps for children and families residing in the Athol Hospital service area.
In conjunction with another hospital, Pender Memorial Hospital successfully implemented the Transitions in Care program. The program provides telehealth for congestive heart failure patients to assist with self-managing cardiac disease, reducing readmissions and encouraging independent living for seniors.
Sanpete Valley Hospital worked with Intermountain Healthcare to create a network that provides appropriate access to behavioral health, working within the community to educate about mental health issues, increase access to care, provide timely access to services and improve follow-up with patients.
McKenzie Health System received recognition for working on key projects such as the Patient Centered Medical Home (PCMH) model to develop a deeper relationship with patients and develop skills to improve patient health through evidence-based medicine techniques to manage chronic disorders.
Estes Park Medical Center (EPMC) was recognized for its work in the areas of care coordination, care management, patient access and prevention and wellness projects. EPMC joined a public-private partnership to form a wellness center that provides an array of services to the community.
Illini Community Hospital has implemented a care coordination program that consolidates management of populations into one seamless system, producing efficiencies that drive improved health outcomes and reduce overall health care spending.