Hospitals participating in the Small Rural Hospital Improvement Program (SHIP) are permitted to make investments in hardware, software, and training that help to participate in or prepare for delivery system reforms such as accountable care organizations (ACOs) other shared savings programs. Created by Centers for Medicare and Medicaid Services, ACOs are groups of physicians, hospitals, and other health care providers, who come together voluntarily to give coordinated high-quality care to the Medicare beneficiaries they serve.
The example activities listed below — from the
FY 2024 SHIP Allowable Investments
(175.07 KB)
— are not intended to be a comprehensive list, but can assist eligible SHIP hospitals in planning and selecting appropriate investments.
For additional clarification, refer to the SHIP Allowable Investments Search Tool and SHIP Frequently Asked Questions (FAQ).
Examples of Accountable Care Organization (ACO) or Shared Savings Investment Activities
| ACO or Shared Savings Investment Activities | Examples of Allowable Activities |
| A. Computerized provider order entry implementation (CPOE) and/or training | Any educational trainings that support use and implementation. |
| B. Pharmacy services training, hardware/ software, and machines (not pharmacists; services or medications) | |
| C. Population health or disease registry training and/or software/hardware | Educational training, or hardware/software to support the development and implementation of a disease registry for care coordination. Software and training for analysis of population health needs by chronic disease or geographic location for care management programs. |
| D. Social determinants of health (SDOH) screening software/training | Software and training for analysis of social determinants of health (SDOH) for improving health outcomes and care management programs. |
| E. Efficiency or quality improvement training or software in support of ACO or shared savings related initiatives | Quality Improvement trainings such as the following: Consider other efficiency or quality improvement trainings or software to address performance issues related to the following: |
| F. Systems performance training in support of ACO or shared savings related initiatives | Hospitals interested in systems performance training should consider adopting a framework approach in transitioning to value-based system planning such as one of the following: |
| G. Telehealth and mobile health hardware/software (not telecommunications) | Training hardware/software that supports the application and implementation of telehealth and/or telemedicine. Tablets and hardware/software investments are allowed if they are used by staff to improve operational efficiencies and telehealth services. |
| H. Community paramedicine hardware/software and training | Community Paramedic Program (CPP) training. If the hospital and/or hospital-owned ambulance units has a formal CPP, then hardware/software can be purchased to support the CPP to reduce inappropriate Emergency Department Use and emergency department and readmissions. However, use of SHIP funding for general EMS equipment is not allowable. |
| I. Health Information Technology (HIT) training for value and ACOs including training, software, and risk assessments associated with cybersecurity | SHIP supports HIT hardware/software and training, including risk assessments for cybersecurity and health equity. |
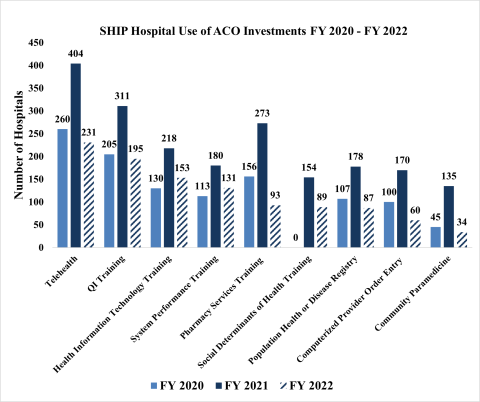
ACO-Specific Investment Activities by SHIP Hospitals, FY 2020 - FY 2022
For more information or for additional support, please contact the SHIP Technical Assistance Team at ship-ta@ruralcenter.org